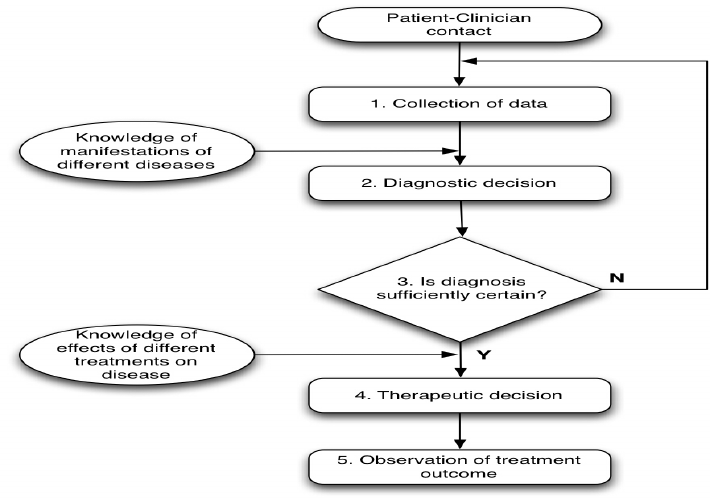
Appropriate clinical decision making has patient care and precise diagnosis at its heart. However, it also balances this against the costs associated with indiscriminate or inappropriate use of diagnostic tests. The risk of possible side effects, improved management and beneficial therapeutic interventions are also assessed.
Clinical decision making is a complex process. It’s based on science but is also somewhat of an art form. No single correct method works for every patient all of the time, however it can be helpful in improving patient care as far as possible.
Clinical decision making has three integrated phases. The first is diagnosis, the second is assessment of severity, and the third is management. Here we’ll look at how they work against the four practical steps healthcare professionals should take.
Step 1: Determining your probabilities
What is the patient’s most likely diagnosis based on their history and symptoms? For instance, if a patient is presenting with a high temperature, fever and cough, your first hypothesis may be COVID-19, bronchitis, or an infection of the upper respiratory tract.
Step 2: Further evaluating the patient to gather more evidence
This would involve additional history taking, followed by a physical exam and a check of the patient’s vital signs. This will help you ascertain if your original hypothesis was correct or not.
Step 3: Updating your probabilities based on the information you’ve obtained
This includes the pre-test probability of any diagnostic test you want to order. Then you’ll need to carefully collect and interpret additional data these diagnostic tests show up. The most likely diagnosis should start to emerge at the top of your differential diagnosis list.
Step 4: Consider an intervention to see whether it crosses your treatment threshold
The more therapeutic benefit (relative to potential harm) is expected in your patient, the lower the treatment threshold should be. If you’re still not sure, you should consider other options, for example additional tests. It may even simply be a case of watching and waiting.
Understanding clinical decision making in more detail
If you’re a primary healthcare professional such as a nurse, paramedic or other practitioner working in acute care, PDUK’s course Clinical decision making & the deteriorating adult in primary care is well worth considering. Offering a solid foundation in the decision-making process, this is a practical course that offers useful tools in effective diagnosis and treatment.
As the course is held online it’s ideal for those looking to fit learning around other work and family commitments. It’s run over 2 days and is worth 14 hours of CPD. However, spaces will be limited so it’s well worth booking up early.